Quitting smoking is best done with the support of a therapist. While nicotine replacement therapies and medications often play a role, a powerful non-pharmacological tool is increasingly being recognized for its effectiveness: Cognitive Behavioral Therapy (CBT).
CBT, at its core, is a structured, goal-oriented approach to psychological treatment. But when applied to smoking cessation, it becomes a sophisticated strategy designed to dismantle the mental machinery that keeps the habit alive.
The Core Idea: Thoughts, Feelings, and Actions
CBT operates on the principle that our thoughts, feelings, and actions are interconnected. In the context of smoking, the act of lighting up isn’t just a physical craving; it’s often the final step in a chain of automatic thoughts and emotional responses.
For example, a stressful day at work might trigger the thought, “A cigarette will calm me down.” This thought leads to feelings of anxiety relief and, finally, the action of smoking. CBT aims to break this chain by identifying and modifying the unhelpful thoughts and behaviors that serve as “triggers.”
How a Session Unfolds
CBT for smoking cessation is typically delivered over several sessions, either individually or in a group setting. It is not a casual chat; it involves active work and strategy building.
First, the therapist and patient establish a precise functional analysis of the smoking habit. This means meticulously tracking when, where, and why the person smokes. It seeks to answer the crucial question: what function does the cigarette actually serve? Is it a social crutch, a mechanism for managing stress, or a way to fight boredom?
Once these triggers are mapped out, the core techniques of CBT come into play:
Cognitive Restructuring: This involves challenging and replacing the nicotine-related beliefs that have been ingrained over years. For instance, the thought “I can’t handle stress without a cigarette” is challenged with evidence and alternative, more constructive coping statements, such as “I can manage stress by taking a short walk or using deep breathing.”
Behavioral Skills Training: Patients are taught concrete strategies to avoid and cope with high-risk situations. This includes stimulus control—changing environmental cues that trigger smoking (like moving an armchair where they always smoked)—and coping skills training, which equips them with alternatives to smoking when a craving hits. This might be a physical activity, a relaxation technique, or a simple distraction method.
Relapse Prevention: This is a crucial final phase. It prepares the individual for inevitable slip-ups or cravings by viewing them not as failures, but as temporary setbacks that can be learned from. Patients develop a tailored “escape plan” for high-risk situations in the future.
Who Benefits and Who Should Be Cautious?
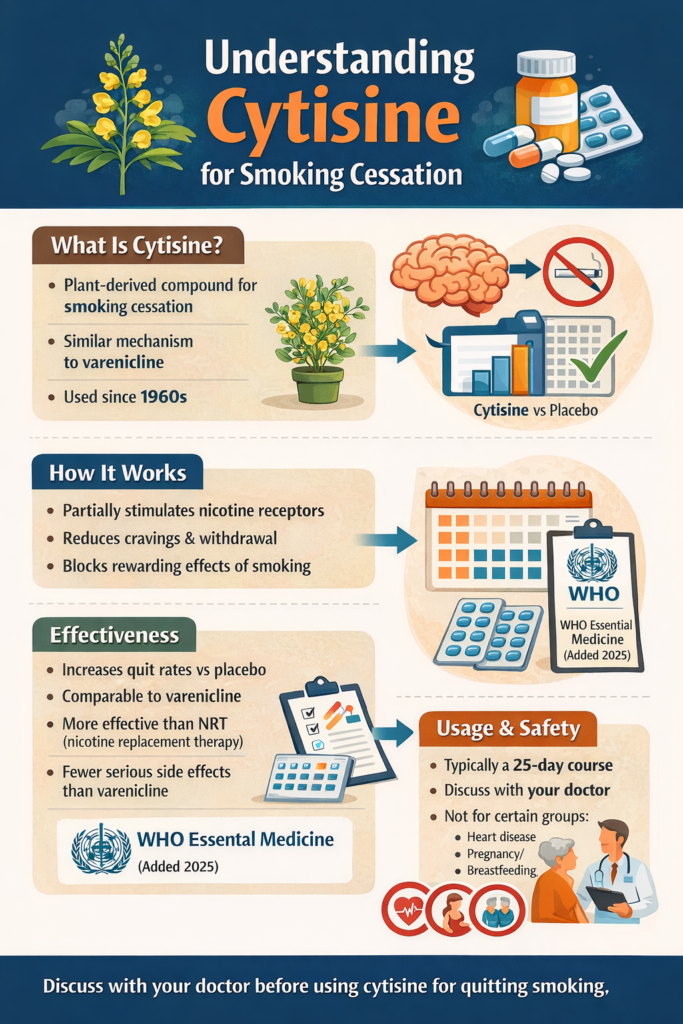
CBT has demonstrated significant effectiveness, particularly when combined with pharmacological aids like Varenicline or Nicotine Replacement Therapy (NRT). Studies show that by addressing both the physical addiction and the psychological dependence, the chances of sustained abstinence are substantially higher.
It is highly suitable for:
- Individuals with strong psychological dependence: Those whose smoking is heavily tied to emotional states, stress, or specific environments.
- Smokers with co-occurring anxiety or depression: CBT is often a first-line treatment for these conditions, making it a powerful dual-purpose tool.
- Those who have tried other methods and relapsed: CBT offers a fresh approach by focusing on the underlying thought patterns that led to the return of the habit.
It may be less suitable for:
- Individuals unwilling to engage in introspection: CBT requires motivation and a willingness to examine one’s own thoughts and challenge long-held beliefs. It is an active process that requires homework and commitment.
Rate this article by clicking on the desired number of stars:
Please use the “Comments” field below to share your experience or suggest improvements to this article.