Living with a partner who smokes often creates tension between concern and respect for personal choice. Pressuring or blaming rarely works, as smoking is tied to routine, identity, and dependence. Productive conversations start with empathy, good timing, and listening, focusing on shared concerns rather than accusations. Lasting change depends on the smoker’s own motivation, supported by patience and mutual understanding. Above all, smoking is an addiction, not a simple habit, and successful quitting often requires support from a health professional as well as encouragement from a partner.
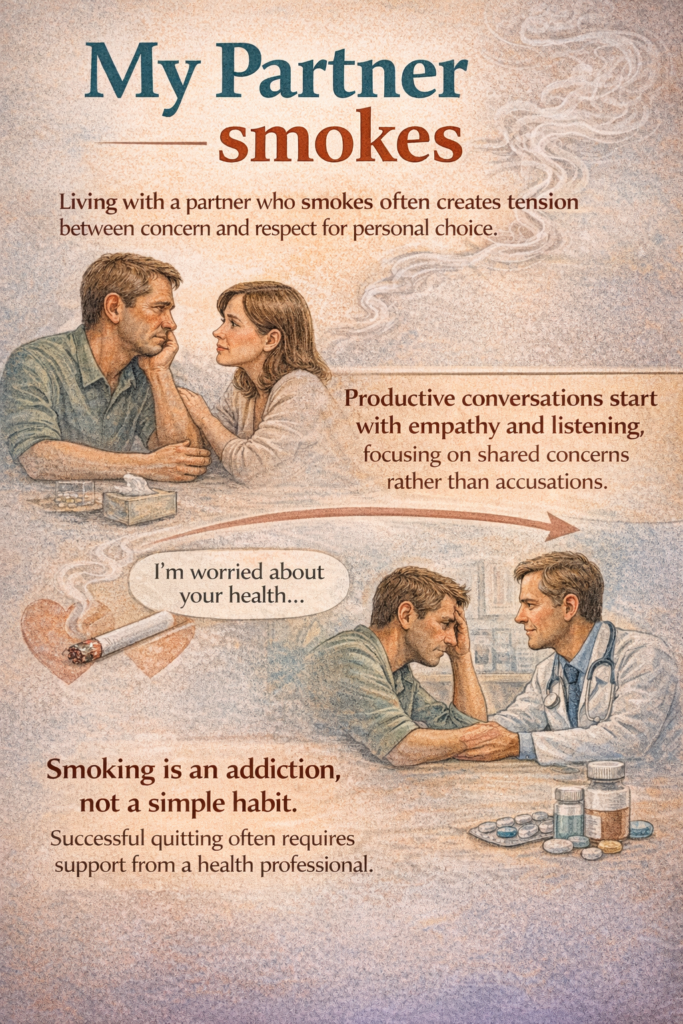
Living with someone who smokes can be complicated. It is rarely just about the smell of tobacco or the smoke lingering in the air. It often touches deeper concerns: health, shared space, future plans, and sometimes fear. Many people find themselves caught between the desire to protect their loved one and the risk of turning every conversation into a source of tension.
Resistance to change is a natural human reaction, and smoking is no exception. For many smokers, cigarettes are tied to routine, stress relief, social moments, and identity. Asking someone to quit can feel, to them, like an attack on personal freedom or a denial of comfort in an already demanding world. This is why pressure, ultimatums, or repeated reproaches so often backfire. They may provoke defensiveness, silence, or even increased smoking.
Starting a conversation requires timing and tone more than arguments. Choosing a calm moment, away from conflict, makes a difference. Speaking from personal feelings rather than accusations helps keep the discussion open. Saying “I’m worried about your health” or “I find it hard to live with smoke at home” invites dialogue, while blame tends to shut it down. Listening matters as much as speaking. Many smokers are already aware of the risks and feel trapped between guilt and dependence.
Effective approaches are rarely dramatic. Small, realistic steps are often better accepted than grand demands. Agreeing on smoke-free spaces, acknowledging attempts to cut down, or simply recognizing how difficult quitting can be can shift the dynamic from confrontation to cooperation. Change is more likely when the smoker feels respected rather than judged.
At the heart of lasting change is inner motivation. No one quits smoking successfully just to please someone else, at least not for long. The decision has to come from within. A partner can help by gently encouraging reflection: What does smoking bring? What does it take away? How might life look without it? These questions open doors without forcing answers.
Mutual support plays a crucial role. Quitting smoking is not a solitary act; it affects daily routines, moods, and relationships. When partners face it together, the burden is lighter. Support may mean patience during irritability, celebrating progress rather than perfection, or adjusting shared habits that trigger smoking. It also means acknowledging that setbacks happen and do not equal failure.
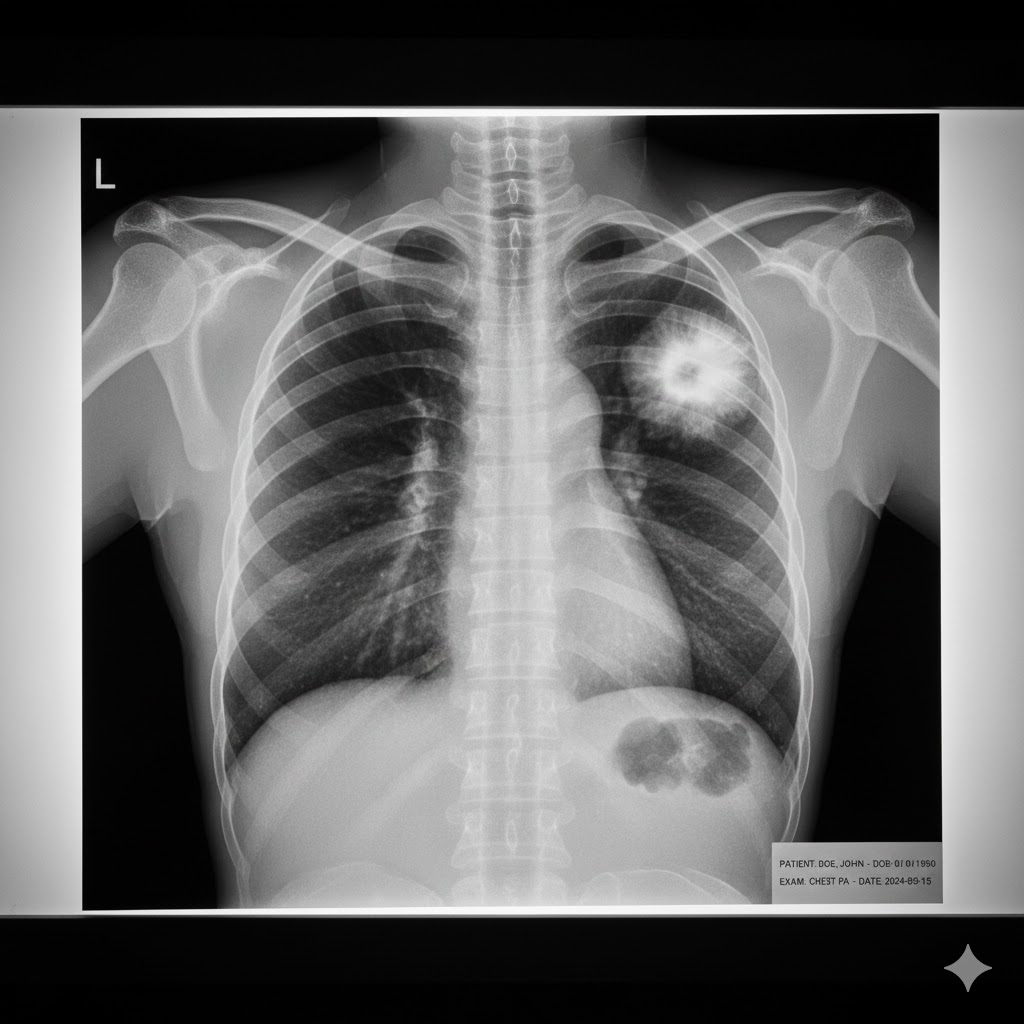
Perhaps the most important point is often overlooked: smoking is not just a habit, it is an addiction. Nicotine changes the brain, creates dependence, and makes quitting far more complex than simple willpower. Treating nicotine addiction as a medical issue rather than a moral weakness changes the conversation. Health professionals are trained to help, with counseling, medications, and strategies that significantly improve the chances of success.
Loving someone who smokes can be frustrating, worrying, and at times exhausting. Yet approaching the issue with empathy, patience, and realism can transform conflict into collaboration. When smoking is understood as an addiction and quitting as a process that deserves support and professional care, the path forward becomes clearer, and more hopeful, for both partners.
Use the ‘Comments’ field below to share your experience on this topic or to suggest improvements to this page.